Introduction of Extracorporeal Shockwave Therapy (ESWT) for Running Injuries

Soft tissue injuries are common to runners and athletes who depend on their legs to get them where they need to go. About 65% of regular runners get hurt each year. It’s estimated that the average runner will sustain one injury for every 100 hours he or she runs.1 When an injury occurs, athletes and weekend warriors are usually looking for solutions to get them back on the road as soon as possible.
What is shockwave?
They are high-energy waves created by sharp changes of pressure in a narrow region, traveling through a medium like air or water. They are normally caused by an explosion or by a body moving faster than sound.2
How does shockwave help tissue?
High energy waves, that can be created via different mechanisms, create a phenomenon referred to as mechanotransduction. In simple terms, it is the process of imparting brief, physical deformation to cells that lead to biochemical changes. These changes have the potential to positively impact pain and tissue repair.3
In some instances, the negative pressure created during the tensile phase of a shockwave creates cavitation bubbles within cells.4 If intense enough, it can lead to disruption of damaged cells which is why shockwave can be classified as a proinflammatory modality.
Disruption of cells can lead to cell death (apoptosis) which triggers a low-level inflammatory response that benefits the process of removal and replacement of damaged tissue. This is another way that shockwave therapy can uniquely assist in treating chronic soft tissue problems.
Terminology
Names that refer to therapeutic shockwave are varied. This can create confusion when trying to investigate this technology. Common names include but are not limited to:
- ESWT: Extracorporeal Shockwave Therapy
- FSW: Focused Shockwave
- EPAT: Extracorporeal Pulsed Activation Therapy
- RPW: Radial Pressure Wave
- AWT: Acoustic Wave Therapy
The list seems to grow by the month as companies try to differentiate their products.
Classification of FSW vs RPW
Generally speaking, there are two primary families of devices under the ESWT umbrella, the focused shockwave (FSW) and radial pressure wave (RPW) devices. While the two waves possess different physical characteristics, they generate similar results when treating various conditions in the musculoskeletal system with equivalent dosing.5, 6
Definition of shockwave components and characteristics
A FSW is a high-intensity, low-frequency (1 to 8 Hz) wave that impacts tissue differently than therapeutic ultrasound (US). Therapeutic shockwaves are non-thermal waves that create mechanotransduction and in some cases cavitation in tissues as deep as 12 cm.4, 7
FSW energy delivery is measured in mJ/mm2 which is referred to as Energy Flux Density (EFD). EFD ranges between 0.01 and 0.55 mJ/mm2 on Chattanooga FSW equipment.8 Preferable dosing ranges exist when treating different conditions. For example, treating with extremely low energy levels (below 0.08 mJ/mm2) has been shown to be ineffective and/or less effective than treating in higher energy ranges.6, 9
On the other end of the spectrum, treating at energy levels >0.60 mJ/mm2 has been shown to be deleterious to tendons.9 Understanding correct dosing parameters and treatment approaches is imperative to achieving consistent results with this equipment.
Interpreting bar pressure vs energy flux density (EFD)
RPW devices are commonly measured in bar pressure. This is likely due to the pneumatic mechanism that generates pressure waves. Bar pressure should ideally be measured at the point where the applicator meets the skin to ensure accurate clinical relevance. 1 bar is equivalent to 14.5 psi. With the correct conversion factors, bar pressure can be converted to EFD. This allows for equivalent dosing parameters to be calculated when comparing RPW and FSW treatments of a given condition. An example of a radial pressure wave is pictured below next to a traditional focused shockwave for ease of comparison. Notice the differences in peak pressure, rate of the wave cycle, as well as the general shape of the 2 waves.

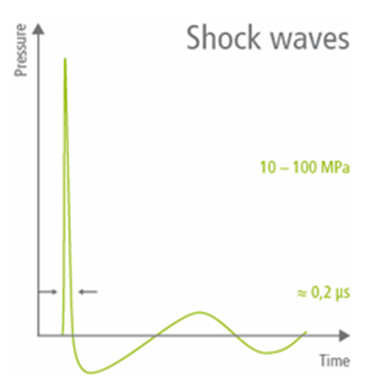
Fig 1. What are shock waves? Physics and Technology. STORZ MEDICAL - The Shock Wave Company. Accessed January 9, 2024. https://www.storzmedical.com/us/physics-and-technology
The physical impact of shockwaves can help improve the environment surrounding recalcitrant problems in muscle, calcific tendons, plantar fasciitis, as well as different connective tissues.
Are all soundwaves the same?
Some clinicians falsely assume that shockwave equipment is similar to therapeutic ultrasound (US) since they both utilize soundwaves. It should be noted that therapeutic ultrasound uses a lower intensity sound wave (20 to 1000 mW/cm2) that is delivered at a higher frequency (0.7 to 3.3 MHz.).10 Therapeutic US waves look like this:

Fig 2. What are shock waves? Physics and Technology. STORZ MEDICAL - The Shock Wave Company. Accessed January 9, 2024. https://www.storzmedical.com/us/physics-and-technology
Continuous US creates thermal effects in tissue by alternating compression and rarefaction of sound waves within tissue. Maximum energy absorption in soft tissue occurs from 2 to 5 cm and intensity decreases as the waves penetrate deeper.10
Hopefully this review will provide some clarity for readers that are looking to better understand how ESWT can help various conditions as well as which device is best suited for a given practice setting.
References
- Running Injuries. Yale Medicine. https://www.yalemedicine.org/conditions/running-injury#:~:text=About%2065%20percent%20of%20regular%20runners%20get%20hurt
- shockwave definition. Bing. Accessed December 18, 2023. https://www.bing.com/search?q=shockwave+definition&cvid=fc98a1ef85b74e16acacd38d178a34da&gs_lcrp=EgZjaHJvbWUqBggAEAAYQDIGCAAQABhAMgYIARBFGDkyBggCEAAYQDIGCAMQABhAMgYIBBAAGEAyBggFEAAYQDIGCAYQABhAMgYIBxAAGEAyBggIEAAYQDIICAkQ6QcY8gcyBwgKEEUY_FXSAQgyMTY5ajBqNKgCALACAA&FORM=ANAB01&PC=U531
- d’Agostino MC, Craig K, Tibalt E, Respizzi S. Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg. 2015;24(Pt B):147-153. doi:10.1016/j.ijsu.2015.11.030
- Fuchs J. Stable vs. Transient Cavitation. CTG Technical Blog. Published January 17, 2019. Accessed December 18, 2023. https://techblog.ctgclean.com/2019/01/stable-vs-transientcavitation/#:~:text=Basically%2C%20the%20cavity%20is%20created%20but%20the%20contents
- Schroeder AN, Tenforde AS, Jelsing EJ. Extracorporeal Shockwave Therapy in the Management of Sports Medicine Injuries. Current Sports Medicine Reports. 2021;20(6):298-305. doi:https://doi.org/10.1249/JSR.0000000000000851
- Schmitz C, Császár NB, Milz S, et al. Efficacy and safety of extracorporeal shock wave therapy for orthopedic conditions: a systematic review on studies listed in the PEDro database. Br Med Bull. 2015;116(1):115-138. doi:10.1093/bmb/ldv047
- RPW User Manual. https://enovis-medtech.eu/media/storage.djoglobal.eu/en_US/Documents/Support_documents/IFU_13-28670_US_Rev_A_Intelect_RPW_2_DIGITAL_Final.pdf
- Focus Shock Wave User Manual. https://www.djoglobal.eu/media/storage.djoglobal.eu/en_US/Documents/Documents_2023/13-00061-US_RevE_USA_IFU,_FOCUS_SHOCKWAVE-EN.pdf
- Rompe JD, Kirkpatrick CJ, Küllmer K, Schwitalle M, Krischek O. Dose-related effects of shock waves on rabbit tendo Achillis. A sonographic and histological study. J Bone Joint Surg Br. 1998;80(3):546-552. doi:10.1302/0301-620x.80b3.8434
- Uddin SMZ, Komatsu DE, Motyka T, Petterson S. Low-Intensity Continuous Ultrasound Therapies—A Systematic Review of Current State-of-the-Art and Future Perspectives. J Clin Med. 2021;10(12):2698. Published 2021 Jun 18. doi:10.3390/jcm10122698



